Tracheostomy care in the hospital setting presents unique challenges that require careful navigation to ensure patient safety, comfort, and optimal outcomes. From initial placement to ongoing management, healthcare professionals must be equipped to address various complexities associated with tracheostomies. Here, we explore key challenges and strategies for effectively managing tracheostomy care within the hospital environment.
Understanding Tracheostomy Care
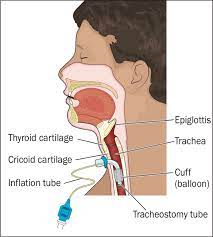
A tracheostomy is a surgical procedure that involves creating a direct airway access through an incision in the neck into the trachea. This intervention is often necessary for patients requiring long-term mechanical ventilation, those with upper airway obstructions, or those who need assistance with secretion management.
Key Challenges
1. Initial Placement and Complications:
- Proper placement of the tracheostomy tube is critical to avoid complications such as tube misplacement, bleeding, or damage to surrounding structures.
- Immediate post-placement care requires close monitoring for signs of respiratory distress, bleeding, or tube dislodgement.
2. Infection Prevention:
- Tracheostomy sites are susceptible to infection, including cellulitis, pneumonia, and tracheitis, necessitating rigorous infection control measures.
- Proper hand hygiene, sterile technique during tube changes, and regular site care are essential for reducing infection risk.
3. Airway Management:
- Maintaining a patent airway is paramount in tracheostomy care, necessitating vigilant monitoring for signs of airway obstruction, mucus plugging, or tube occlusion.
- Suctioning, humidification, and regular tube checks are vital components of airway management.
4. Communication and Swallowing:
- Tracheostomy tubes bypass the vocal cords, impairing speech and swallowing in patients.
- Implementing communication strategies such as speaking valves, communication boards, or alternative communication methods is crucial for patient engagement and psychological well-being.
- Dysphagia management protocols should be implemented to prevent aspiration and ensure safe swallowing.
5. Weaning and Decannulation:
- Successful weaning from mechanical ventilation and eventual decannulation require careful assessment of respiratory function, swallowing ability, and overall medical stability.
- Multidisciplinary collaboration involving respiratory therapists, speech-language pathologists, and physicians is essential in facilitating the weaning process.
Strategies for Effective Tracheostomy Care
1. Standardized Protocols:
- Implementing evidence-based protocols for tracheostomy care, including insertion, maintenance, and weaning procedures, promotes consistency and reduces variability in practice.
2. Interdisciplinary Team Collaboration:
- Establishing a multidisciplinary tracheostomy care team comprising nurses, respiratory therapists, speech-language pathologists, and otolaryngologists fosters comprehensive patient management and enhances communication.
3. Ongoing Education and Training:
- Providing regular education and training sessions for healthcare providers on tracheostomy care guidelines, emergency procedures, and complication management ensures competency and enhances patient safety.